Collateral Damage: Reversing the Trends of Pandemic-Triggered Mental Illness
By Lisa Rue, PhD., cliexa Senior Advisor Adolescent Behavioral Health
Findings from a 2021 study of cliexa’s holistic screening (cliexa-OPTIONS) for adolescents and young adults confirms early suspicions regarding mental health issues among adolescents and young adults. The collateral damage resulting from lockdowns during the Covid-19 national response has been devastating, with young people struggling to cope with a range of issues, including how to manage negative feelings of depression, along with anxiety and thoughts of suicide.
Independent research presented this month by Dr. William Merchant from the Department of Applied Statistics and Research Methods (ASRM) and Dr. Stephen Wright from the Department of Applied Psychology and Counselor Education (APCE) at the University of Northern Colorado found dramatic increases in the frequency of patients and clients (ages 14-24 years) dealing with a mental health challenge. The percentages are outlined in Figure 1.
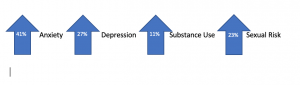
Figure 1. Percentages of UNC Students Exhibiting Various Mental Health Issues (N=202)
Parents and clinicians are facing difficulties in supporting these adolescents and young people. The continuum of mental health and wellness fluctuates regularly, increasing or decreasing depending on individual resiliency and support. While little can be done about individual genetic predisposition to depression or anxiety, certain measures can support young people by building resiliency or protective factors when increased risk is identified. Parents and clinicians can encourage resiliency and protective factors by asking a few targeted questions, such as:
Do you have a trusted adult, friend or family member that you can chat with? If not, can we think of someone together? Sometimes just being able to talk to someone about how you are feeling helps us cope.
Tell me some good things about yourself? What are some areas that you know you do well in that you can continue to develop? Let’s make a plan to spend more time building your skills and confidence in these areas.
Do you think people are respecting you? How do you think you can get people to respect your position and listen to your concerns? Sharing your concerns without getting angry will help communicate your concerns and validate
What makes you happy? What can you do to spend more time on things that make you happy?
What are some of your goals in the next 6 months? Two years? What are some steps you can take to meet those goals?
How has the pandemic affected your behavior and actions toward others? What can we control with respect to how we treat others during this difficult time?
A new resource available now, is the Dibble Institute’s new website for teens called Me and My Emotions (MeandMyEmotions.org), is a timely resource. Young people will find a wealth of information that they can use on their own to build resiliency, mindfulness skills, and improve mental wellness.
If mental health struggles sound familiar, remind your loved ones that they are not alone, and that life will eventually get back to normal. During this temporary struggle, it’s important to avoid using alcohol and other drugs to cope. Instead, focus on increasing your protective factors to decrease risks and create balance.
For more information about this study and its benefits, click here.
cliexa’s CEO & Founder, Mehmet Kazgan, selected as one of “30 Best Leaders to Watch in 2019” by The Silicon Review
News, Press Coveragecliexa’s Founder and CEO, Mehmet Kazgan, is rated as one of the “30 Best Leaders to Watch in 2019” Mehmet was featured in an article highlighting his success as an entrepreneur, and business owner. Mehmet founded cliexa in late 2015 and has been working diligently to grow the company. Mehmet sat down with the Silicon Review team to discuss his experience as a leader in business, and healthcare technology.
Here is a snippet from the article:
“What is your greatest fear, and how do you manage fear?”
“My greatest fear is to over-promise and under-deliver, in any form, within a business or non-business related context. I manage fear by acknowledging it and facing it when the time comes.”
“What were the biggest initial hurdles to building your business and how did you overcome them?”
“Convincing others about my entrepreneurial approach and vision was one of the biggest hurdles. Validating the concept and demonstrating the outcomes was one of the ways I worked to overcome them.”
To read the full article, click HERE.
cliexa wins Department of Health & Human Services: Agency for Healthcare Research and Quality’s Step Up App Challenge.
Digital Health, Mobile Health, News, Patient Experience, Patient Reported Outcomes, Press Releasecliexa advances to Phase 2 of the AHRQ Step Up App Challenge
Chronic Care Management, Digital Health, News, Patient Engagement, Patient Reported Outcomes, Press Coverage, Press Releasecliexa is one of 10 companies out of 50+ advancing to Phase 2 of the Agency for Healthcare Research and Quality (AHRQ)‘s Step-Up App Challenge with the “goal of developing an app that integrates standardized patient-reported outcomes (PRO) data into clinical care and research.”
For Phase 2 of the Step Up App Challenge, cliexa will design, develop, and demo our application using the FHIR technical specifications and PROMIS® resources for patient-reported outcomes with the hope to be selected as one of the three winners, who will get the opportunity to test their product in nine practice settings affiliated with MedStar Health in Washington, DC.
Read the blog announcing the 10 semifinalists from Director of the AHRQ, Gopal Khanna, M.B.A: https://www.ahrq.gov/news/blog/ahrqviews/stepup-challenge-finalists.html
Check out our portfolio of patient-reported outcomes applications: cliexa Mobile
cliexa Announces Partnership with Bluenet Technologies!
News, Press Coverage, Press ReleaseBluenet and cliexa are excited to announce their new partnership, combining their strengths to develop new ways to improve patient care through technology.
This is an exciting time for the healthcare industry. With new technologies and innovative solutions being developed, we are on the cusp of a whole new era in healthcare. Bluenet and cliexa are leading the charge. They are working together to bring innovation to healthcare.
Bluenet is known for its expertise in cloud-based solutions, while cliexa is leading change in transforming patient-reported data into actionable insights for healthcare providers through the power of artificial intelligence. This partnership will allow both companies to combine their strengths and develop new ways to improve patient care. Healthcare providers can expect to see improved operational efficiencies, enhanced decision support, and better clinical outcomes from this collaboration.
Bluenet’s Managing Director, Sukru Tutak, states that “Bluenet’s mission has always been about delivering high-quality data solutions for its customers. Therefore, we were immediately impressed by cliexa’s focus on creating the best integrated patient care platform in the healthcare industry by combining quality, volume, and speed of data. Bringing these two great organizations together and letting them work toward common goals made perfect sense.”
Mehmet Kazgan, CEO and Founder at cliexa, states, “We are excited to partner with Bluenet, who has a strong background in Business Intelligence and Digital Transformation. Not only are we strengthening our resource expansion opportunity, we are also broadening our health information technology and interoperability consulting approach with Bluenet’s years of experience.”
The future of healthcare is looking very bright, and we are honored to be a part of it. We encourage you to check out what cliexa is doing; their solutions are changing the game for healthcare providers and patients alike. Together, we are ushering in a new era of healthcare innovation – one that will benefit everyone involved. Stay tuned for more updates as we work together to bring innovative solutions to healthcare!
————————–
About Cliexa:
cliexa is an end-to-end virtual health platform that provides clinicians a complete understanding of real-time patient data. cliexa removes the barriers and inaccuracies in data collection, empowering clinicians to provide personalized care. cliexa’s patented technology powered by artificial intelligence is validated with industry leaders like Mayo Clinic and the American College of Cardiology.
About Bluenet:
Founded in 2004 in Tampa, Florida, Bluenet provides its clients with services in the areas of Data & Analytics (BA), IT Talent Management, Managed IT Services, and Digital Transformation. We have distinguished ourselves in the marketplace by consistently delivering the highest-quality services that positively impact our client’s growth, competitiveness, and operational efficiency. We consider every client engagement as a strategic and long-term partnership.
cliexa Partners with Lucem Health to bring its Opioid Use Disorder Prediction Platform to the Point of Care
Blog, News, Press Coverage, Press ReleaseDenver, CO – cliexa announces a strategic partnership with Lucem Health providing expert support and an innovative platform to help deploy and commercialize cliexa’s Opioid Use Disorder Prediction Platform in clinical settings.
Pain management teams must overcome significant complexity to deliver effective clinical care to opioid patients, including, managing the interplay of multiple, chronic medical conditions, behavioral health issues, and intricate medication management. This onerous process places unnecessarily high cognitive loads-on clinicians that increase the risk of burnout.
cliexa platform empowers pain management teams with the right data, at the right time, directly within the workflow of electronic medical records, freeing up clinic staff’s cognitive space, and enabling clinicians to make the best choice for the patient sitting in front of them.
cliexa recently completed Mayo Clinic Platform-Accelerate and announced its Opioid Use Disorder Prediction Model trained with de-identified patient data provided by the Mayo Clinic Platform. cliexa also worked with technology experts from Google to ensure the highest standards of transparency and minimize bias.
cliexa and Lucem Health will work together and identify technical enablement and commercialization processes as well as anticipated ROI for cliexa’s predictive model in clinical settings. Lucem Health will assist cliexa by adding further insights to end users, taking cliexa’s AI model, and putting it in context for the appropriate end users.
“Right after our recent launch of Opioid Use Disorder Machine Learning Algorithms, Lucem Health partnership will be further verification of our platform, especially for commercialization stage and improve our delivery with industry experts. We feel extremely lucky and excited for this partnership opportunity.” Said, Mehmet Kazgan, Founder and CEO of cliexa.
“The Innovation Collaborative helps AI/ML and Digital Health innovators create, deploy, and commercialize clinical AI solutions that transform care,” says Sean Cassidy, CEO, Lucem Health. “Our partnership with cliexa is further testament of our continually growing partner network, and the wealth of possibilities it provides to our customers.”
“We are very pleased to see cliexa, the graduate of the first Accelerate cohort, receive support from Lucem, a Mayo Clinic Platform portfolio company,” says Eric Harnisch, vice president, Partner Programs, Mayo Clinic Platform.
About cliexa:
cliexa, Denver-based digital health firm, developed an end-to-end virtual health platform that provides clinicians a complete understanding of real-time patient data. cliexa removes the barriers and inaccuracies in data collection, empowering clinicians to provide personalized care. cliexa partnered with industry-leading organizations like Mayo Clinic and the American College of Cardiology to validate its patented technology powered by AI to change patients’ lives.
About Lucem Health:
Lucem Health™, launched with Mayo Clinic along with investing partners Commure (a General Catalyst company) and Rally Ventures, empowers healthcare visionaries to quickly bring AI-powered insights to the point of care. Digital health innovators develop transformative clinical solutions and advance them from the bench to the bedside to the front lines of healthcare on a single integration platform. Visionary clinical leaders deploy novel data and insights seamlessly into clinical workflows while ensuring that clinicians trust, adopt, and see value in them. For more information, visit www.lucemhealth.com.
cliexa joins Mayo Clinic Platform Accelerate!
Blog, Digital Health, News, Press Coverage, Press Releasecliexa joined Mayo Clinic Platform_Accelerate, an immersive program for health tech startups as part of its initial cohort of participating companies.
The program offers cliexa access to Mayo Clinic experts in regulatory, clinical, technology and business domains with a focus on AI model validation and clinical readiness. Technology experts from Google and Epic also will provide workshops.
"Health tech startups are critical contributors to the cycle of innovation," says John Halamka, M.D., president of Mayo Clinic Platform, a strategic initiative to improve health care through insights and knowledge derived from data. "We are excited to collaborate with these innovators to solve some of the most complex problems in medicine today."
cliexa will:
"We are helping participants take a crucial step in their growth trajectory by providing startups with a disciplined focus on model validation and clinical readiness to show product value," says Eric Harnisch, Vice President of Partner Programs for Mayo Clinic Platform. "The program is integral to our Mayo Clinic Platform mission to enable new knowledge, new solutions and new technologies that improve patients' lives worldwide."
Read more at Mayo Clinic News Network Press Release here.
###
About Mayo Clinic Platform
Founded on Mayo Clinic's dedication to patient-centered care, Mayo Clinic Platform enables new knowledge, new solutions and new technologies through collaborations with health technology innovators to create a healthier world. To learn more, visit the Mayo Clinic Platform website.
About Mayo Clinic
Mayo Clinic is a nonprofit organization committed to innovation in clinical practice, education and research, and providing compassion, expertise and answers to everyone who needs healing. Visit the Mayo Clinic News Network for additional Mayo Clinic news.
Help Teens Experience Healthy Relationships This Valentine’s Day
BlogValentine’s Day can make many people feel left out. Teens and young adults are particularly susceptible to harmful relationship beliefs and peer pressure. They take in messages like, “If you love me, you will . . . .” Fill in the blank with any conditional requirement. This raises a red flag. Young people are learning about the many con games and romantic masks that create toxic relationships. Your patients may sense that their relationship is imbalanced in terms of commitment. If relationships are a problem for your patients or clients, consider the way OPTIONS can help them make better choices. Inform patients and clients that they can always rewind a relationship, take a time-out from a relationship, or start over completely!
Recent findings from the University of Northern Colorado indicate that 18% of the sample of participants aged 14 – 24 years of age (N=109) have low satisfaction with their decision to have sex. In addition, 69% do not use risk reduction strategies correctly.
This Valentine’s Day make a commitment to helping young people learn how to establish authentic intimate relationships. Ask your patients questions such as, “Is sex everything you thought it would be?” “Have you ever thought about taking a time-out from sex in order to recalibrate your decisions about intimate relationships?” One client’s decision to take a time-out from sex exemplifies the challenges young adults may experience with intimate relationships:
I realized that I had nothing to show for the numerous sexual encounters that I had had. And I began to hate the fact that I had so frivolously given away the most intimate and sacred parts of myself. Instead of finding acceptance and love I found loneliness and a broken heart and I realized that in actuality I didn’t feel any more beautiful and I didn’t feel any more valuable. Instead, I felt misunderstood, insignificant and empty. – Female, Age 21
Timeouts, rewinds, and relationship do-overs create intentionality, reducing ambiguity and increases the use of risk reduction strategies in future relationships. School and community-based relationship education support knowledge and skills that help young people pursue healthy relationships. Clinicians, educators and parents have crucial roles in helping teens and young adults think differently about their sexual choices. The digital app cliexa-OPTIONS fosters effective and brief clinical interventions between providers and patients.
In addition, a recent meta-analysis found relationship education improves communication skills and reduces unhealthy relationship beliefs. School-based relationship education such as the evidence-based Healthy Futures program supports relationship skills for middle school students. Young people deserve the best relationships. This Valentine’s Day help teens and young adults take advantage of new approaches.
For more information on cliexa-OPTIONS research, contact Dr. William Merchant at the University of Northern Colorado: William.Merchant@unco.edu.
Collateral Damage: Reversing the Trends of Pandemic-Triggered Mental Illness
Blog, Digital Health, Public HealthCollateral Damage: Reversing the Trends of Pandemic-Triggered Mental Illness
By Lisa Rue, PhD., cliexa Senior Advisor Adolescent Behavioral Health
Findings from a 2021 study of cliexa’s holistic screening (cliexa-OPTIONS) for adolescents and young adults confirms early suspicions regarding mental health issues among adolescents and young adults. The collateral damage resulting from lockdowns during the Covid-19 national response has been devastating, with young people struggling to cope with a range of issues, including how to manage negative feelings of depression, along with anxiety and thoughts of suicide.
Independent research presented this month by Dr. William Merchant from the Department of Applied Statistics and Research Methods (ASRM) and Dr. Stephen Wright from the Department of Applied Psychology and Counselor Education (APCE) at the University of Northern Colorado found dramatic increases in the frequency of patients and clients (ages 14-24 years) dealing with a mental health challenge. The percentages are outlined in Figure 1.
Figure 1. Percentages of UNC Students Exhibiting Various Mental Health Issues (N=202)
Parents and clinicians are facing difficulties in supporting these adolescents and young people. The continuum of mental health and wellness fluctuates regularly, increasing or decreasing depending on individual resiliency and support. While little can be done about individual genetic predisposition to depression or anxiety, certain measures can support young people by building resiliency or protective factors when increased risk is identified. Parents and clinicians can encourage resiliency and protective factors by asking a few targeted questions, such as:
Do you have a trusted adult, friend or family member that you can chat with? If not, can we think of someone together? Sometimes just being able to talk to someone about how you are feeling helps us cope.
Tell me some good things about yourself? What are some areas that you know you do well in that you can continue to develop? Let’s make a plan to spend more time building your skills and confidence in these areas.
Do you think people are respecting you? How do you think you can get people to respect your position and listen to your concerns? Sharing your concerns without getting angry will help communicate your concerns and validate
What makes you happy? What can you do to spend more time on things that make you happy?
What are some of your goals in the next 6 months? Two years? What are some steps you can take to meet those goals?
How has the pandemic affected your behavior and actions toward others? What can we control with respect to how we treat others during this difficult time?
A new resource available now, is the Dibble Institute’s new website for teens called Me and My Emotions (MeandMyEmotions.org), is a timely resource. Young people will find a wealth of information that they can use on their own to build resiliency, mindfulness skills, and improve mental wellness.
If mental health struggles sound familiar, remind your loved ones that they are not alone, and that life will eventually get back to normal. During this temporary struggle, it’s important to avoid using alcohol and other drugs to cope. Instead, focus on increasing your protective factors to decrease risks and create balance.
For more information about this study and its benefits, click here.