Collateral Damage: Reversing the Trends of Pandemic-Triggered Mental Illness
By Lisa Rue, PhD., cliexa Senior Advisor Adolescent Behavioral Health
Findings from a 2021 study of cliexa’s holistic screening (cliexa-OPTIONS) for adolescents and young adults confirms early suspicions regarding mental health issues among adolescents and young adults. The collateral damage resulting from lockdowns during the Covid-19 national response has been devastating, with young people struggling to cope with a range of issues, including how to manage negative feelings of depression, along with anxiety and thoughts of suicide.
Independent research presented this month by Dr. William Merchant from the Department of Applied Statistics and Research Methods (ASRM) and Dr. Stephen Wright from the Department of Applied Psychology and Counselor Education (APCE) at the University of Northern Colorado found dramatic increases in the frequency of patients and clients (ages 14-24 years) dealing with a mental health challenge. The percentages are outlined in Figure 1.
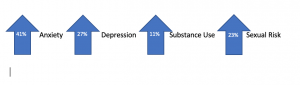
Figure 1. Percentages of UNC Students Exhibiting Various Mental Health Issues (N=202)
Parents and clinicians are facing difficulties in supporting these adolescents and young people. The continuum of mental health and wellness fluctuates regularly, increasing or decreasing depending on individual resiliency and support. While little can be done about individual genetic predisposition to depression or anxiety, certain measures can support young people by building resiliency or protective factors when increased risk is identified. Parents and clinicians can encourage resiliency and protective factors by asking a few targeted questions, such as:
Do you have a trusted adult, friend or family member that you can chat with? If not, can we think of someone together? Sometimes just being able to talk to someone about how you are feeling helps us cope.
Tell me some good things about yourself? What are some areas that you know you do well in that you can continue to develop? Let’s make a plan to spend more time building your skills and confidence in these areas.
Do you think people are respecting you? How do you think you can get people to respect your position and listen to your concerns? Sharing your concerns without getting angry will help communicate your concerns and validate
What makes you happy? What can you do to spend more time on things that make you happy?
What are some of your goals in the next 6 months? Two years? What are some steps you can take to meet those goals?
How has the pandemic affected your behavior and actions toward others? What can we control with respect to how we treat others during this difficult time?
A new resource available now, is the Dibble Institute’s new website for teens called Me and My Emotions (MeandMyEmotions.org), is a timely resource. Young people will find a wealth of information that they can use on their own to build resiliency, mindfulness skills, and improve mental wellness.
If mental health struggles sound familiar, remind your loved ones that they are not alone, and that life will eventually get back to normal. During this temporary struggle, it’s important to avoid using alcohol and other drugs to cope. Instead, focus on increasing your protective factors to decrease risks and create balance.
For more information about this study and its benefits, click here.