Last week, over 12,000 public health professionals flocked to San Diego for the 75-degree weather, ocean views, and the most significant public health conference in the U.S, the American Public Health Association’s Annual Meeting and Expo. Two large buildings downtown were dedicated to housing deep dive conversations about, among other things, tobacco use, obesity, women’s health, racial inequity in health and the most cutting-edge research in the field. In reflection, I had three takeaways from the conference about the role and use of digital health in public health.
#1. Health technology and its benefits are not largely understood in its application to the public health community.
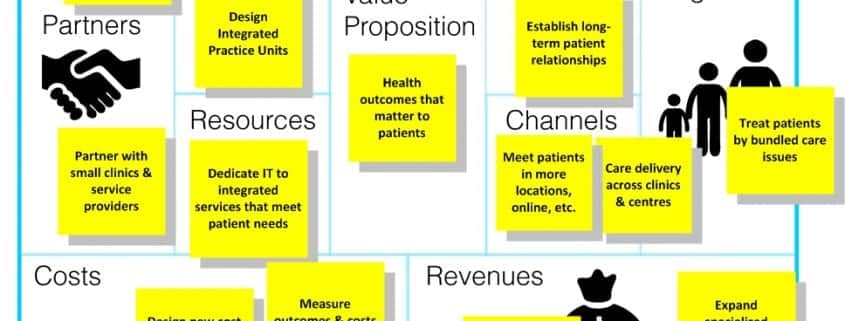
Many times, throughout the conference I found myself reiterating the value of a health platform for clinical, research or evaluation processes. Many people I spoke to had a genuine interest but weren’t sure how technology could optimize their work. In reality, many public health programs and projects are researched and evaluated using patient-reported data. Imagine digitizing that process so patients can participate through an application on their phone; imagine the impact that would have on response rates and loss-to-follow-up. Imagine the benefits of pushing routine surveys to patient’s phone instead of having to call to do scheduled evaluations. Not to mention the equitable distribution of programs and interventions across diverse populations, rural populations and those who have transportation barriers that technology can help address. In public health we operate in a world of outcomes, without being able to show outcomes we don’t see funding renewals, patient participation fades away, and programs fail. Health technology provides a way for researchers and evaluators to track outcomes in real time.
#2. UX/UI can be a major make-or-break when looking at making a tool that applies to diverse or vulnerable populations.
My first event was a meeting in a small room with other health technology professionals discussing the process that they’ve undergone to get health technology recognized as a section at APHA. In this room, we considered the impacts on research, evaluation, follow up, data visualization and overall patient experience. One of the most impactful conversations that I had was with a social worker who embraced technology as a tool for diverse or vulnerable populations. She emphasized how user interface and user experience can shape program success in diverse and vulnerable populations. She encouraged me to reach out to individuals who interact directly with the specific population when designing products to be used in public health settings. Only if the patient or client is engaged with the tool, can we see the successes or obtain accurate information for physicians, for researchers, or health program evaluators. A crucial point when considering Take Away #1, and the importance of highlighting tangible outcomes over time.
#3. There is “data overload” in public health.
This conference had some of the country’s top experts in health, with rows of poster projects, all with their own calculated data sets backing the findings that they were at APHA to present. Some will likely be published while others will remain in the researcher’s computer with little other exposure. I spoke to individuals who were collecting health data, payor data, and policy data, and all were positioning their data sets in different areas independent of each other despite their overwhelming connectivity. With the rate that new studies are conducted, data changes so quickly so even systematic reviews and meta-analyses become outdated far too quickly. There is an opportunity to leverage technology to collect a real-time outcomes database to ensure the hard work that researchers do to make correlations and identify patterns is not lost in the data black hole. Entities such as the CDC, NIH and WHO do an excellent job of collecting and displaying related data sets for public use, however the time that it takes to gather data often puts the data sets months to years behind the times. There is a significant opportunity for technology to lend to this real-time collection process.
Overall, the themes of APHA for me centered around how much opportunity there is to impact the way public health programs are research, delivered and evaluated through the use of digital health. These conversations were inspiring and exciting but also demonstrated how much we still have to do to fully optimize the work that we do in the public health field.