cliexa joined Mayo Clinic Platform_Accelerate, an immersive program for health tech startups as part of its initial cohort of participating companies.
The program offers cliexa access to Mayo Clinic experts in regulatory, clinical, technology and business domains with a focus on AI model validation and clinical readiness. Technology experts from Google and Epic also will provide workshops.
"Health tech startups are critical contributors to the cycle of innovation," says John Halamka, M.D., president of Mayo Clinic Platform, a strategic initiative to improve health care through insights and knowledge derived from data. "We are excited to collaborate with these innovators to solve some of the most complex problems in medicine today."
cliexa will:
- Work with data science experts to delineate AI model requirements.
- Check for fairness and bias in their AI models.
- Gain understanding of Food and Drug Administration clearance pathways.
- Access de-identified Mayo Clinic patient data in a secure environment.
- Conduct model validation with guidance from data science experts.
- Plan clinical validation studies, such as clinical simulation or clinical trials.
- Explore eligibility to partner with Mayo Clinic Platform.
"We are helping participants take a crucial step in their growth trajectory by providing startups with a disciplined focus on model validation and clinical readiness to show product value," says Eric Harnisch, Vice President of Partner Programs for Mayo Clinic Platform. "The program is integral to our Mayo Clinic Platform mission to enable new knowledge, new solutions and new technologies that improve patients' lives worldwide."
Read more at Mayo Clinic News Network Press Release here.
###
About Mayo Clinic Platform
Founded on Mayo Clinic's dedication to patient-centered care, Mayo Clinic Platform enables new knowledge, new solutions and new technologies through collaborations with health technology innovators to create a healthier world. To learn more, visit the Mayo Clinic Platform website.
About Mayo Clinic
Mayo Clinic is a nonprofit organization committed to innovation in clinical practice, education and research, and providing compassion, expertise and answers to everyone who needs healing. Visit the Mayo Clinic News Network for additional Mayo Clinic news.
Valentine’s Day can make many people feel left out. Teens and young adults are particularly susceptible to harmful relationship beliefs and peer pressure. They take in messages like, “If you love me, you will . . . .” Fill in the blank with any conditional requirement. This raises a red flag. Young people are learning about the many con games and romantic masks that create toxic relationships. Your patients may sense that their relationship is imbalanced in terms of commitment. If relationships are a problem for your patients or clients, consider the way OPTIONS can help them make better choices. Inform patients and clients that they can always rewind a relationship, take a time-out from a relationship, or start over completely!
Recent findings from the University of Northern Colorado indicate that 18% of the sample of participants aged 14 – 24 years of age (N=109) have low satisfaction with their decision to have sex. In addition, 69% do not use risk reduction strategies correctly.
This Valentine’s Day make a commitment to helping young people learn how to establish authentic intimate relationships. Ask your patients questions such as, “Is sex everything you thought it would be?” “Have you ever thought about taking a time-out from sex in order to recalibrate your decisions about intimate relationships?” One client’s decision to take a time-out from sex exemplifies the challenges young adults may experience with intimate relationships:
I realized that I had nothing to show for the numerous sexual encounters that I had had. And I began to hate the fact that I had so frivolously given away the most intimate and sacred parts of myself. Instead of finding acceptance and love I found loneliness and a broken heart and I realized that in actuality I didn’t feel any more beautiful and I didn’t feel any more valuable. Instead, I felt misunderstood, insignificant and empty. – Female, Age 21
Timeouts, rewinds, and relationship do-overs create intentionality, reducing ambiguity and increases the use of risk reduction strategies in future relationships. School and community-based relationship education support knowledge and skills that help young people pursue healthy relationships. Clinicians, educators and parents have crucial roles in helping teens and young adults think differently about their sexual choices. The digital app cliexa-OPTIONS fosters effective and brief clinical interventions between providers and patients.
In addition, a recent meta-analysis found relationship education improves communication skills and reduces unhealthy relationship beliefs. School-based relationship education such as the evidence-based Healthy Futures program supports relationship skills for middle school students. Young people deserve the best relationships. This Valentine’s Day help teens and young adults take advantage of new approaches.
For more information on cliexa-OPTIONS research, contact Dr. William Merchant at the University of Northern Colorado: William.Merchant@unco.edu.
Collateral Damage: Reversing the Trends of Pandemic-Triggered Mental Illness
By Lisa Rue, PhD., cliexa Senior Advisor Adolescent Behavioral Health
Findings from a 2021 study of cliexa’s holistic screening (cliexa-OPTIONS) for adolescents and young adults confirms early suspicions regarding mental health issues among adolescents and young adults. The collateral damage resulting from lockdowns during the Covid-19 national response has been devastating, with young people struggling to cope with a range of issues, including how to manage negative feelings of depression, along with anxiety and thoughts of suicide.
Independent research presented this month by Dr. William Merchant from the Department of Applied Statistics and Research Methods (ASRM) and Dr. Stephen Wright from the Department of Applied Psychology and Counselor Education (APCE) at the University of Northern Colorado found dramatic increases in the frequency of patients and clients (ages 14-24 years) dealing with a mental health challenge. The percentages are outlined in Figure 1.
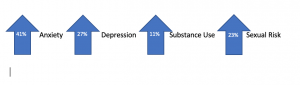
Figure 1. Percentages of UNC Students Exhibiting Various Mental Health Issues (N=202)
Parents and clinicians are facing difficulties in supporting these adolescents and young people. The continuum of mental health and wellness fluctuates regularly, increasing or decreasing depending on individual resiliency and support. While little can be done about individual genetic predisposition to depression or anxiety, certain measures can support young people by building resiliency or protective factors when increased risk is identified. Parents and clinicians can encourage resiliency and protective factors by asking a few targeted questions, such as:
Do you have a trusted adult, friend or family member that you can chat with? If not, can we think of someone together? Sometimes just being able to talk to someone about how you are feeling helps us cope.
Tell me some good things about yourself? What are some areas that you know you do well in that you can continue to develop? Let’s make a plan to spend more time building your skills and confidence in these areas.
Do you think people are respecting you? How do you think you can get people to respect your position and listen to your concerns? Sharing your concerns without getting angry will help communicate your concerns and validate
What makes you happy? What can you do to spend more time on things that make you happy?
What are some of your goals in the next 6 months? Two years? What are some steps you can take to meet those goals?
How has the pandemic affected your behavior and actions toward others? What can we control with respect to how we treat others during this difficult time?
A new resource available now, is the Dibble Institute’s new website for teens called Me and My Emotions (MeandMyEmotions.org), is a timely resource. Young people will find a wealth of information that they can use on their own to build resiliency, mindfulness skills, and improve mental wellness.
If mental health struggles sound familiar, remind your loved ones that they are not alone, and that life will eventually get back to normal. During this temporary struggle, it’s important to avoid using alcohol and other drugs to cope. Instead, focus on increasing your protective factors to decrease risks and create balance.
For more information about this study and its benefits, click here.
Dr. Dhaliwal, who recently joined cliexa’s executive management team will be leading strategic growth at cliexa. Dr. Dhaliwal, is a physician entrepreneur, has been serving as CEO of Momentum Healthcare Staffing, board member of two VC funds and other healthcare startups. Dr. Dhaliwal also served as the Associate Medical Director of Prognos Health. With his innovative approach and passion in healthcare technology, Dr. Dhaliwal as a practicing physician is highly optimistic about putting a dent on today’s healthcare challenges by partnering with cliexa.
“As a physician and executive, I am excited to be a member of cliexa family. cliexa is truly an innovative solution to not only increase clinical efficiency but also to improve reimbursement within institutions. It will be a great journey to work with cliexa staff and advisors to grow this one stop shop solution, providing a complete platform for patient journey.” said Dr. Dhaliwal.
cliexa since the inception in late 2016, expanded its solutions offering, intelligent patient triage and onboarding, integrated EMR solutions, quality and compliance add-ons and remote patient monitoring. In June 2021, cliexa and American College of Cardiology announced the launch of cliexa-PULSE, device and EMR agnostic patient engagement and remote patient monitoring platform that leverages patient-centered data with multiple co-morbidities. cliexa uses patented clinical data processing algorithms (USPTO Patent# 10628555: evidence-based data collection, processing and indexing algorithms) and now leveraging American College of Cardiology’s proprietary risk algorithms for cardiovascular conditions.
“With Dr. Dhaliwal’s leadership in growth strategy, combined with Dr. Kowalcyzk’s clinical and business guidance, cliexa will be taking a big step in onboarding new customers and expanding its footprint with current health system contracts” said Mehmet Kazgan, Founder and CEO of cliexa.